The Heart :
- Is a muscle about the size of your fist.
- Weighs approximately one pound.
- Is located behind and slightly to the left of the breastbone.
- Pumps about 5 quarts (4.7 liters) of blood every minute or 1800 gallons (6768 liters) of blood every day.
The function of the heart is to circulate blood throughout the body.
- Pumping blood through the lungs removes carbon dioxide and refreshes the blood with oxygen.
- The oxygenated blood is pumped to the body to provide oxygen and nutrients,
and to remove waste products.
A healthy heart beats steadily and rhythmically at a rate of about 60 to 100 beats per minute when at rest (normal sinus rhythm). During strenuous exercise, the heart can increase the amount of blood it pumps up to four times the amount it pumps at rest, within only a matter of seconds.
The heart’s structure has four chambers with one-way flaps called valves. The atria are the upper chambers and they receive blood that is being returned to the heart. The right atrium receives blood with little oxygen because the blood has already circulated throughout the body delivering oxygen and nutrients.
The left atrium fills with newly oxygenated blood returning from the lungs. When the atria pumps (contract), they push the blood through valves (tricuspid and mitral) into the relaxed ventricles. When the ventricles contract, the right ventricle pumps blood through the pulmonary valve into the lungs. The left ventricle pumps blood through the aortic valve to the body, including the heart (through coronary arteries). This continuous cycle of synchronized contractions is driven by the heart’s electrical system.
CORONARY ARTERIES : LIFELINES OF THE HEART
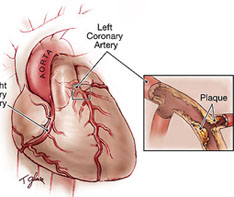
Although the heart is bathed in blood, it cannot derive its own nutrition from the blood it is continuously pumping. For its own oxygen and nutrients, the heart depends on blood from 3 arteries. These coronary arteries arise from the aorta and include the right coronary artery (RCA) and the left main coronary artery (LMCA) which in turns divides in to two branches: the left anterior descending coronary artery (LAD) and the left circumflex coronary artery (LCx). The LMCA is the most important artery of the heart supplying almost 70-80 % of blood to the heart’s muscle. Of this the LAD accounts for approximately 50% of the heart’s blood supply, and the LCx for 20-30%. The remaining 20-30% of the heart’s blood supply comes from the RCA. An occlusion (blockage) of the LMCA is almost always fatal. LAD blockage is next in seriousness, and results in severe damage to the heart. Occlusions of the RAC and LCx, or smaller side branches of any of the coronary arteries are usually less dangerous and result in a heart attack of variable size and severity, depending on the artery, which is blocked.
ROSCLEROSIS: THE PROCESS OF HARDENING OF THE CORONARY ARTERIES.
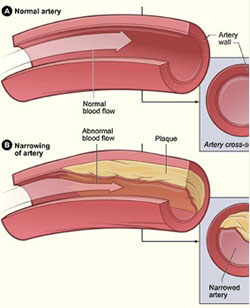
A HEALTHY CORONARY ARTERY : A healthy artery is normally smooth-walled. Blood flows through it easily without any turbulence. Healthy coronary arteries provide the heart with sufficient blood both during rest and when the heart’s demands are raised e.g. during exercise.
ATHEROSCLEROSIS : This is scientific name for the process of hardening of the coronary arteries. The process of atherosclerosis is a universal process of ageing (like the age related whitening of our hair). It occurs in everyone to some extent with advancing age. Atherosclerosis begins from early childhood by deposition of cholesterol and other fatty substances (called fatty plaques) in the wall of the arteries. This process goes on during an individual’s life, slowly in some and faster in others.
A NARROWED AETERY : With time, these fatty plaques grow in size and harden, which may lead to a narrowing of the coronary arteries, somewhat like scale formation on the inside of a metal water pipe. When the coronary arteries become narrowed by more than 70%, the amount of oxygen reaching the heart muscle may not be enough to meet its demands. This inadequacy of blood supply becomes especially significant when the heart must work harder as during exercise, stress, after food etc. It is then that the heart muscle cries out in pain, which is called angina pectoris.
A BLOCKED ARTERY : If blood flow is completely blocked in the artery by a plaque, or a blood clot (thrombus) forming within the narrowed artery, the heart muscle supplied blood by this artery does not receive any blood and starts to die. This leads to a heart attack. The blockage of the artery can occur as the result of a gradual build up of cholesterol within the artery over several years. A slowly developing occlusion may give time for the heart to compensate for the blockage by the development of small alternate pathways called collaterals. These collaterals are a boon for the heart, and may even prevent a heart attack when this slowly narrowing artery finally occludes. Another way that an artery may get blocked is when a small and often insignificant plaque becomes unstable and ruptures. Rupture of this unstable plaque may occur due to stress, excitement, exercise, or sudden rise of blood pressure. Plaque rupture results in a loss of the normal smooth lining of the arterial wall, which in turn induces thrombus formation. Since the occlusion in this case is abrupt, there is no opportunity for collaterals to develop and the resultant heart attack is invariably larger than if the occlusion had been more gradual.
RISK FACTORS OF CORONARY ARTERY DISEASE
– NON-MODIFIABLE (THAT YOU CANNOT CHANGE):
– FAMILY HISTORY
– AGE
– GENDER (MALE and FEMALE)
MODIFIABLE (THAT YOU CAN CHANGE) :
- SMOKING (Directly responsible for at least 20% deaths from heart diseases)
- CHOLESTEROL
- HIGH BLOOD PRESSURE
- DIABETES (60% Deaths from heart attack)
- OBESITY: A 2000 study reported that men who have waist that measure more than 36 inches & have triglyceride levels (more than 200 mg%) are at high risk of developing heart diseases within 5 years.
- EATING HABITS
- SEDENTARY LIFESTYLE (twice as likely to have heart attack)
- STRESS/DEPRESSION
TYPE OF PERSONALITY :
- Impatient, always in a hurry
- Appears tensed, restless, preoccupied
- Tends to get angry quickly
- Strives for perfection
- Dominating, competitive
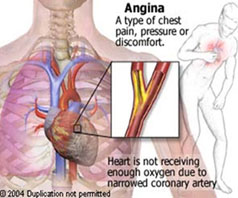
SYMPTOMS ANGINA PECTORIS
Angina is a direct consequence of atherosclerosis (hardening) of the coronary arteries. Atherosclerosis is a slowly developing process in which cholesterol and other fatty substances are deposited in the wall of the arteries, somewhat like scales forming on the inside of a pipe. Atherosclerosis is a normal ageing process (like the whitening of hair) and occurs in everybody to some extent with growing age. However, in some people, this process is more pronounced and the inside of the artery gets narrowed, impeding normal blood flow. This is the stage when one may experience warning symptoms in the form of chest pains (angina pectoris).
WHAT IS ANGINA PECTORIS?
Angina is the heart muscle’s complaint that it is not getting enough oxygen. Angina literally means ‘choking’. Angina pectoris is the term used to denote the suffocating discomfort in the chest owing to the heart receiving less oxygen due to a narrowed coronary artery.
Location of the pain
The typical pain in the left side of the chest radiating to the left arm, neck and back almost confirms angina.
Trigger factors for the pain
Angina pain is very typically related to physical exertion and is relieved by rest. However, there are exceptions to this pattern.
Types of pain
Most people complain of heaviness or tightness in the middle of their chest. Some of them may feel uneasiness or suffocate. Diabetic patients may not experience the typical chest pain and often complain of uneasiness or breathlessness. This is basically because they lose the pain sensation due to nerve damage caused by diabetes.
Severity of pain
Based on the severity, angina is classified into
Class- 1, where the patient gets the symptom after severe exertion like running, walking uphill, carrying weight.
Class- II, where the patient can walk up to 1-2 Km without symptoms
Class- III, angina is brought on by slight exertion.
Class IV, is when angina occurs at rest.
Importance of Early detection of Heart disease
Fifty million Indians suffer from one or more types of cardiovascular disease, the most common of them being Coronary Heart Disease (CHD). Not all are patients. Most of them are individuals who go about their day-to-day activities not knowing that they suffer from heart disease. Unfortunately, expensive and often life-threatening invasive procedures have been the mainstay for the prevention and management of CHD. Early diagnosis and treatment of CHD is presently not being given the focus it actually needs.
Q: Why should I know about Heart Disease and the methods to detect it, when I am healthy?
A: Because for 50% of people who have heart disease, heart attack may be the first symptom and 50% of them may not survive the first attack. Definitely not the best way to find out!
India is all set to face a Heart Disease Epidemic by 2010. The WHO estimates that India will have 100 million people with Coronary Heart Disease (CHD). On an average, CHD occurs at least 10-15 years earlier among Indians than among Western population, indicating that more and more people below 40 years are developing heart disease. Recent studies among Indians have shown that, apart from having the highest rate of incidence, Indians also have the highest rates of death due to heart attacks, when compared to Americans, Europeans, Chinese and Japanese.
Unless we detect heart disease early and take appropriate steps, we cannot prevent a heart attack.
Q: Are Indians more prone to developing Heart disease?
A: The answer appears to be – Yes. Genetic predisposition could account for difference between CHD occurrence in Indians and other populations. Adding to that, are factors like wrong diet, lack of physical activity and high levels of stress. Some of the reasons postulated for this higher incidence are
- Indians have higher levels of triglycerides and Lipoprotein A, as compared to other populations.
- Indians are naturally prone to develop Diabetes, since they have a tendency towards abdominal obesity.
- Indians have a higher incidence of underweight children due to poor maternal nutrition during pregnancy.
Interestingly, the type of CHD occurring among Indians also seems to be different. In the West, most cases are single blocked arteries, whereas in India double and triple blocked arteries appear to be common. That’s why the death rate is higher when there is a heart attack. Another reason could be that our arteries are smaller.
Moreover, there are no standardized programs for prevention of Heart disease in India like those from malaria or tuberculosis. Countries like Australia, Canada and US have experienced significant decline in the rate of cardiovascular disease due to public education, screening programs and preventive measures.
Q: What do we mean by screening for Heart Disease?
A: Screening means sorting out from a large population of apparently healthy people, those who are likely to have the disease. By early detection of the heart disease and subsequent action, we can ensure that no major cardiac events like chest pain or heart attack occur.
Q: What is the purpose of screening test for Coronary Heart Disease?
A: In many patients, the first symptom of CHD is myocardial infraction or sudden death, with no preceding chest pain as a warning. For this reason, doctors perform screening tests to detect signs of CHD before any serious medical events occur. Screening tests are of particular importance for patients with risk factors for CHD. These risk factors include a family history of CHD at relatively young age, an abnormal serum cholesterol profile, cigarette smoking, elevated blood pressure and diabetes mellitus.
Q: How do we known if a test is accurate or not?
A: The accuracy of any test is measured by two parameters called sensitivity and specificity.
Sensitivity of a test indicates its ability to accurately diagnose those who have the disease. A test with 100% sensitivity means if 100 people who have heart disease undergo the test, the test is positive in all the 100 cases. In a test with low sensitivity for e.g. in IMI whose sensitivity is only 65% the test will be positive only in 65 people of the 100 people with heart disease who underwent the test. So the remaining 35 people, who underwent the test, will go back thinking they are normal, and will not know they have heart disease till they have a chest pain or heart attack. Specificity of a test refers to its ability to correctly rule out those who do not have the disease and minimizes the chance of being false positive. If a test has less sensitivity, the chances of being further investigated with invasive procedures are high.
It is important for a screening test to have high sensitivity and high specificity.
Investigation of Heart Disease
Several tests diagnose possible heart disease. The choice of which and how many tests it takes to know the answers vary. These include patient’s risk factors, history of heart problems, current symptoms and the doctor’s interpretation of these factors. People being evaluated for possible heart disease are usually given a simple test first. Then more complicated ones may be used, if needed. Specific tests depend on the patient’s particular problem and their physician’s assessment.
Q: What happens if I am found to have signs of blockages?
A: When mild blockages are detected, the recommended therapy is risk factor modification such as cholesterol lowering and cessation of smoking if applicable, and use of aspirin and certain vitamins such as vitamins E and C. Other lifestyle interventions like nutritional modifications, stress control measures and exercises would be aggressively instituted.
By doing all these, we are ensuring that though the person has developed blockages, the blood flow to the heart improves and that he does not suffer a heart attack.
Q: My doctor tells me that a particular test is Non-invasive. What does he mean by that?
A: Non-invasive tests are those that don’t involve inserting needles, instruments or fluids into the body.
Some examples of non-invasive tests used for detection of heart disease are
- Resting electrocardiogram (ECG or EKG)
- Chest X-ray
- Holter monitor (Ambulatory electrocardiogram)
- Echocardiogram
- Exercise stress test or Stress ECG or Tread Mill Test or TMT
- 3D Cardiovascular cartography scans.
- Computed Tomography (CT) scans – Ultra fast CT. Electron Beam CT, Spiral CT.
- Magnetic resonance Imaging (MRI)
- Magnetic resonance Angiography (MRA)
Q: What are other imaging tests that are available?
A: The following tests are invasive and require a needle to be punctured in the vein.
- Stress test.
- PET test. MUGA scan
- Thallium stress test
- Pharmacological
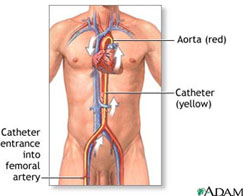
The following tests may require insertion of a catheter
- Trans-esophageal echocardiogram (TEE)
- Cardiac catheterization – also known as Coronary Angiography (CAG)
- Intravascular ultrasound.
- Tests for detection of Heart Disease Chest x – ray

– ECG AND STRESS ECG (TMT) ECG
– Stress ECG
– Echocardiogram
– Ultra fast CT scans
– Coronary Angiography
Test during Acute chest pain or chest discomfort
Q: How does a doctor evaluate those with chest discomfort?
A:1. Medical history, including relevant risk factors for coronary atherosclerosis
2. Physical examination
3. Electrocardiogram.
4. Blood tests
